

Story by
MEGAN TROTTER, HALEY MORELAND
Photos by SHANE DUNLAP
TribLive
Sept. 10, 2024
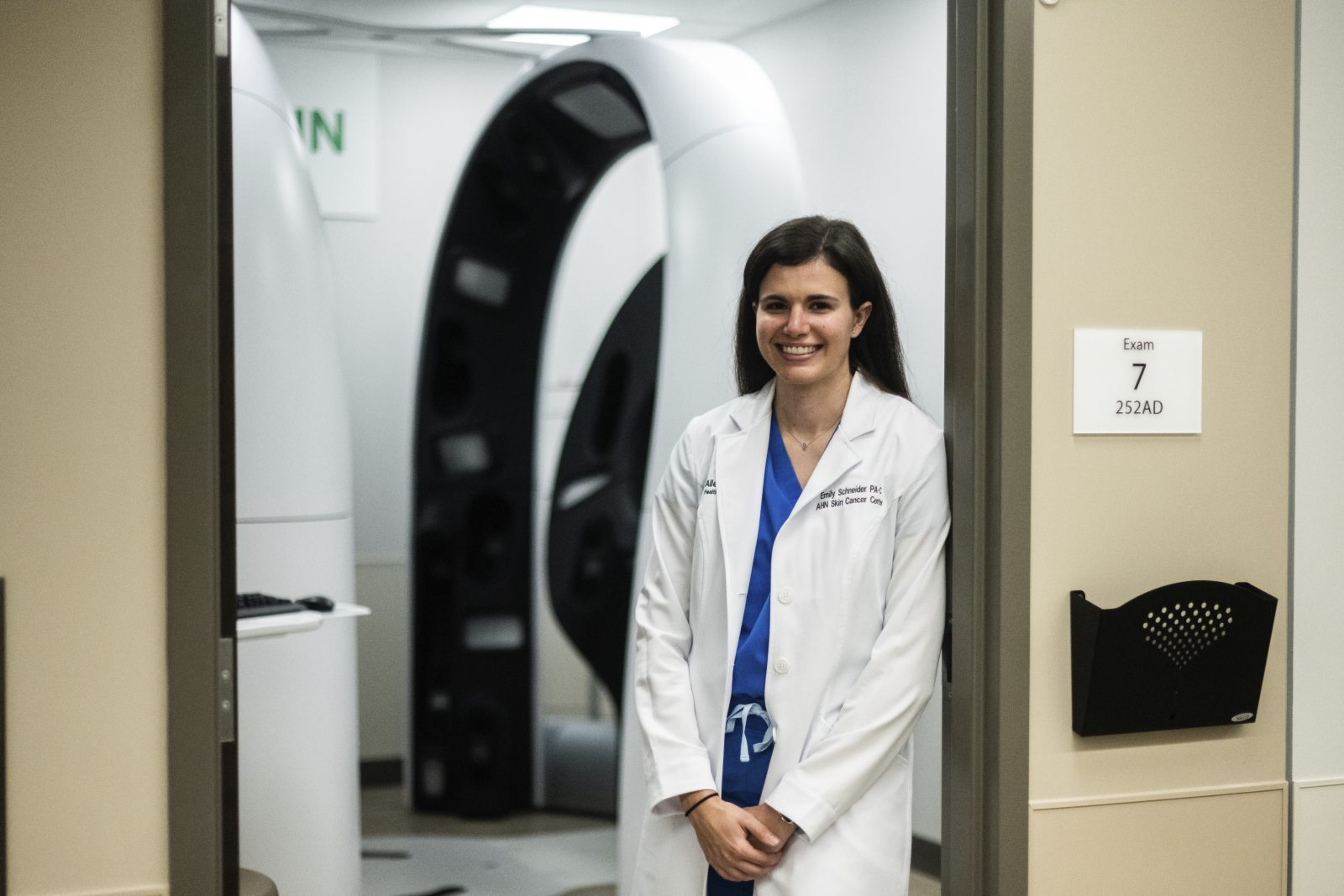
Emily Schneider uses artificial intelligence at work for six hours a day, twice a week.
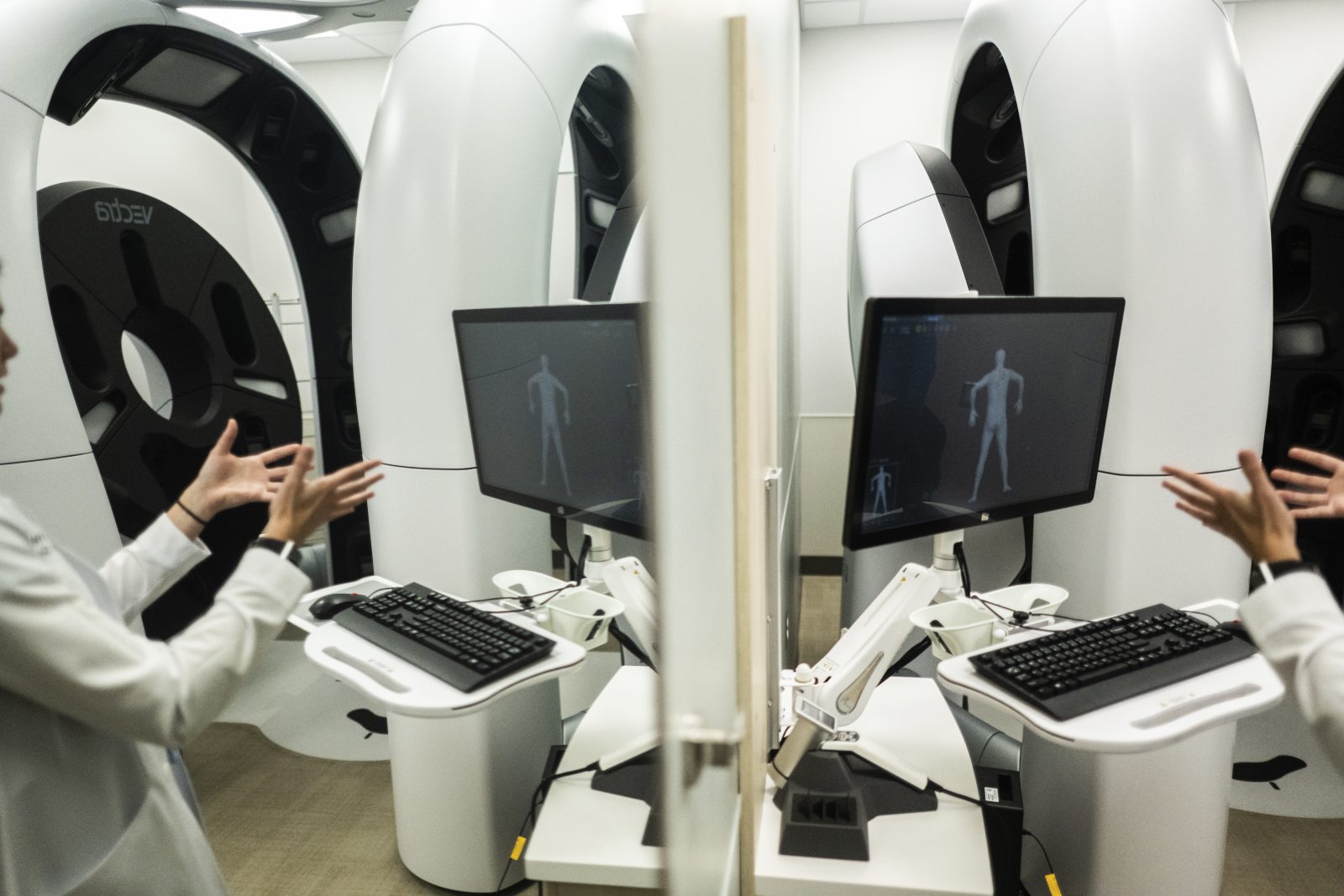
As a physician assistant at West Penn Hospital, it’s her job to man Vectra, a 3D imaging system intended to capture signs of skin disease.
That algorithm the machine uses is an example of artificial intelligence. It uses a vast database of information and applies it to each photograph, identifying potential problems far faster than any human could. It’s one of the many ways AI is being used in medicine to improve patient care.
While the patient plants their feet at the center of the machine, Vectra takes images using 92 cameras installed in the various pods that make up its curving structure.
Those images are then transferred to a computer and analyzed by an algorithm that scores each spot’s risk on a scale from zero to 10. This scale is called the Dermoscopy Explainable Intelligence Score, or DEXI score.
Once the photos have been analyzed and the patient’s records are sent to a specialist, Schneider’s work is done. Each scan takes about an hour, so she can do up to 12 scans a week.
Not only is the process quick, but Schneider said it’s also more effective for identifying changes in skin condition over time.
“I think it’s definitely making an improvement,” Schneider said. “I think it’s just adding to the patient experience.”
Katrina Barger, 38, of Churchill, was the first person to step inside the machine. She was diagnosed with melanoma in 2011, at age 26.
“It was definitely shocking,” Barger said of the cancer diagnosis. “When you’re young, you never really think you’re going to get cancer.”
She had been able to manage her melanoma by attending regular doctor and dermatologist appointments, keeping out of the sun and protecting her skin with sunscreen, but Vectra took her health care a step further.
“I was very impressed because it was able to locate every mole on my body,” Barger said.
Barger has had 30 melanoma spots removed — one of them was detected by Vectra. Vectra also found three other atypical cells on Barger’s skin. She has been inside of the Vectra machine twice, once in October 2023 and again in June.
“It’s available to anyone who wants to use it and make an appointment,” Barger said.
The machine isn’t covered by insurance. A scan costs $250.
Right now, West Penn Hospital is the only hospital in Pittsburgh with AI technology like Vectra. However, according to a 2023 report by Morgan Stanley, 94% of hospitals nationwide were implementing or planning to implement AI technologies.
At Allegheny Health Network, new technologies are being developed and implemented daily. So far, more than 300 providers at AHN have started using AI.
Ashis Barad, a physician who serves as AHN’s chief digital information officer, said the health system started using AI to record and summarize health visits. This new technology, called ambient listening, is intended to shorten the time it takes to file medical records.
Sunday
• The technology is ubiquitous, causing reason for optimism about its impact but concerns about its consequences
• Who are the founding fathers of AI? / What are the different kinds of AI?
Monday
• How AI is being used for finance and investing
Wednesday
• AI in the news; how it impacts what you read
Ambient listening uses an audio recording from the health visit and transcribes it in real time before transforming the recording into a summary. This summary is then edited and approved by a physician before being stored.
Barad said it takes doctors 16 minutes, on average, to file medical records after a health visit. Ambient listening technology can dramatically reduce that time and gives doctors more time for other things, such as spending time with patients.
“We hope that doctors also get to take time where they say … I want a refreshment break (or) I need to use the bathroom,” Barad said. “You think these are simple things, but sometimes when you’re in the throes of (the) clinic, I know plenty of doctors that have waited hours to just go get a drink because they just have so many patients waiting for them.”
Other hospitals such as Penn Medicine and UPMC also have begun using ambient listening in their buildings to help doctors focus on face-to-face interactions with patients.
“A lot of doctors are feeling a sense of burnout, and it’s because of the work that needs to be done … (and) the increasing demands of us to correspond with patients,” said William Hanson, chief medical information officer for Penn Medicine.
Chris Carmody, chief technology officer and senior vice president of UPMC, said system hospitals have implemented nine electronic health record systems.
“It’s shifting our nurses, our doctors away from doing the documentation, having it automatically done so they can focus on a patient,” Carmody said.
While AI has been cutting down on doctors’ time charting, it also has begun to help predict patient behavior and risk factors.
Researchers at Penn Medicine at the University of Pennsylvania Medical System and Penn State University are implementing AI programs that predict people’s risk of infection and disease.
Dr. Liu Dajiang, a health sciences professor and director of artificial intelligence and medical informatics at Penn State’s college of medicine, said doctors are using AI to determine someone’s genetic risk score.
“A lot of people are lucky to be born with some genetic mutations that protect them from developing disease, regardless of their lifestyle,” Dajiang said. “The idea for these algorithms is to figure out what are the protective variants and how they function, so that we can develop a drug that mimics those.”
Using AI, Dajiang said it will become possible to use medical records to quickly conduct DNA sequencing, a practice that can pinpoint genetic disorders. DNA sequencing cost billions of dollars at the beginning of the 21st century, but with AI technologies, prices could drop to a few hundred dollars per patient.
AI also can cut the time between diagnosis and treatment in some cases.
UPMC Enterprises recently created Realyze Intelligence Inc. to match cancer patients with clinical trials at their first visit, helping patients start treatment sooner, Carmody said.

AHN doctors and patients are free to opt out of using ambient listening during health visits. Barad said the health system is working to understand what makes patients uncomfortable with the implementation of AI in their health services.
“We’re spending a whole lot of time to understand how our community feels about AI,” Barad said. “Do they want to know every time AI is used in their health care decisions, or is it one of those things where I expect you to use it?”
At AHN hospitals where AI is used, Barad said, consent forms are given out at the front desk. Verbal consent is sought throughout health care visits where AI technology is being used.
“We’re still at a handful of patients that say no,” Barad said. “Based on data in our communities, most patients are saying, ‘Hey, if that makes you be a better doctor and you spend more time with me and I get to see you, talk to you, then I get it.’”
Schneider said her patients have had no issues with Vectra’s image processing algorithm.
“A lot of people have really embraced it,” she said.
At Independence Health, Chief Information Officer Roger Lutz said the system is cautiously introducing AI into its network to streamline the process of submitting claims to insurance companies.
“Not a very exciting area of health care, but … it is complex,” Lutz said. “With the right technologies, it becomes more effective.”
Still, while Lutz said there are benefits to incorporating AI into medicine, he said Independence Health is holding off on using more AI technologies for now.
“It holds a lot of promise and, for us, it’s just the offerings that are on market right now aren’t a good fit for us just yet,” Lutz said.
Despite some hesitation, others are looking forward to see how AI technologies may impact health care in the future.
“I don’t think AI is going to replace people by any means. I think we see it as a very opportunistic way to help and create efficiencies in health care,” Carmody said. “We can improve upon the quality of care that we deliver to our patients. That’s the ultimate goal. It’s really less about the technology.”
Megan Trotter is a TribLive staff writer. She can be reached at mtrotter@triblive.com. Haley Moreland is a TribLive staff writer. You can reach Haley at hmoreland@triblive.com.
