Erin Wheeler has always known she was at high risk for skin cancer.
A kidney transplant, combined with fair skin from her Irish heritage, put skin cancer on her radar at age 10.
Some three decades later, Wheeler, a senior career consultant at the University of Pittsburgh, is a quasi-regular for Mohs surgery at UPMC St. Margaret Dermatology in Harmar.
“The first time I had Mohs was five years ago on my face,” said Wheeler, 45, of Pittsburgh’s North Oakland section. “I was nervous, of course.
“But I cannot speak highly enough of the procedure, for as much as someone can enjoy going through something like this.”
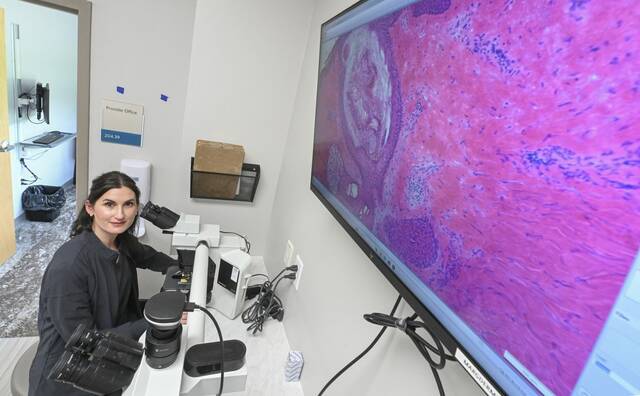
Mohs surgery, named after Dr. Frederic Mohs, who developed the specialized procedure in the 1930s, removes the slimmest layers of skin one by one as a means of sparing healthy tissue.
Surgeons analyze the layers in-office — same day — until there are no signs of cancer.
Demand for Mohs has surged in recent years across the country, in part because of the rising incidences of skin cancer — the diagnosis of nonmelanoma skin cancers in the U.S. increased by 77% between 1994 and 2014.
But people also seek its success.
Mohs is the most effective current treatment for skin cancer, which is diagnosed in more than 9,500 people a day, according to the Skin Cancer Foundation.
There are more than 1 million Mohs procedures each year in the U.S., which is up 10% in the last decade, according to the American Academy of Dermatology.
The demand prompted UPMC St. Margaret’s Dermatology Department to double its surgery space earlier this spring.
The $150,000 project enabled three new procedure rooms, for a total of six, and two new surgical hires, said Kevin MacDonald, vice president of operations.
MacDonald said incidences of skin cancer are increasing because of longer life expectancy, more sun exposure and better detection.
“Mohs surgery is one treatment that minimizes scarring, as patients can attest to,” MacDonald said.
It also has up to a 99% success rate because tumors are removed with acute precision while saving as much healthy skin as possible, according to American College of Mohs Surgery.
Transplant patients, like Wheeler, are at a high risk for skin cancer because of the immunosuppressant drugs. Organ transplant patients are 100 times more likely than the general public to develop squamous cell carcinoma, according to data from the Skin Cancer Foundation.
Dr. Melissa Pugliano-Mauro, UPMC director of dermatological surgery, said the department provides specialized care for solid organ transplant recipients and other immunosuppressed patients.
When Pugliano-Mauro found a suspicious spot above Wheeler’s right eyebrow, Mohs was the obvious choice.
“It’s less invasive, layer upon layer, and doesn’t leave much of a scar if any at all,” Wheeler said. “I was like, ‘Sign me up.’”
Wheeler said the wound healed beautifully and there is no lasting sign of surgery on her forehead.
Since then, she’s had additional Mohs procedures, including a spot on her upper chest in recent weeks. She has hand surgery scheduled this summer.
“I talk to a lot of people about the benefit of Mohs,” Wheeler said.
“The key is that they take less tissue. When it’s not Mohs, it’s like a melon scooper.”