Southmoreland School District is in a legal battle with its teachers union over insurance coverage for prescription weight-loss drugs.
The district has filed a lawsuit in Westmoreland County, asking a judge to overturn an arbiter’s decision that sided with the union.
According to court filings, the district’s decision to stop covering these drugs was based on an independent audit.
The audit claimed their insurer, Highmark, had improperly paid more than $1.9 million in the previous year for specific medications not covered by the district’s plan, including more than $9,000 for weight-loss drugs.
The district claims these drugs were never intended to be part of the existing prescription plan.
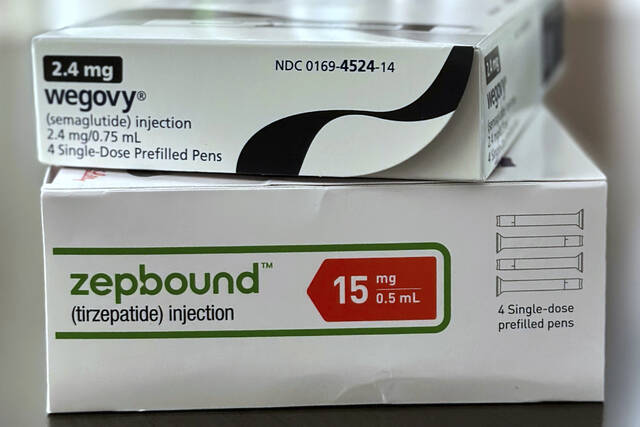
Last October, a consortium that negotiates health care for Westmoreland County’s 17 public school districts voted to stop future payments for drugs whose primary purpose is weight loss, such as Wegovy and Zepbound.
However, drugs with similar formulas, such as Ozempic and Mounjaro, remain covered if prescribed for other medical conditions, such as diabetes, according to court documents.
The arbitration ruling ordered Southmoreland to resume coverage for the weight-loss drugs if they were prescribed for other health-related purposes.
This ruling, however, does not apply to union members in other school districts.
Court documents included with the Southmoreland lawsuit show 510 participants in Westmoreland County school districts’ health plans were prescribed weight-loss drugs during the 2023-24 school year. Of those, 410 participants filled prescriptions for drugs that are now excluded.
In its lawsuit, Southmoreland argues the arbiter’s decision is incorrect. The district claims the ruling was based on the testimony of five teachers who stated they were prescribed the drugs for other ailments, including high blood pressure, elevated cholesterol and thyroid cancer.
“Neither the district nor the association nor the arbitrator have the ability to make medical determinations as to what employees should have coverage under the plan and what employees should not have coverage under the plan. No testimony was elicited at the time of the hearing, and none of the parties are experts in the medical/pharmaceutical field,” according to the lawsuit.
The district also claims covering these drugs could increase health insurance costs by 10%. It claims existing documentation supports its decision to halt payments.
Conversely, the teachers union contends the exclusion is an improper alteration of the negotiated health care plan, which is in effect until 2029. Teachers claim they were forced to stop using the medications in January because they could no longer afford the out-of-pocket costs, and that their health has since deteriorated.
Highmark declined to comment on the lawsuit.
Spokesman Aaron Bilger in an emailed statement said the insurer does not mandate clients to exclude weight-loss drugs from health care plans.
“Payment for covered benefits, including covered weight-loss drugs, is subject to Highmark’s assessment of medical necessity and appropriateness as set forth in medical policy,” Bilger wrote.
He said Highmark determines medical policy for its self-insured clients.
“Medical policies, including those applicable to weight-loss medications, change from time to time as, among other things, our assessment of clinical effectiveness, safety and efficacy can change following ongoing review. This is standard prudent industry practice.”
Last year, the health care provider announced a revision to limit weight-loss drugs from its standard benefits package because of excessive costs.
“We are striving to provide the most value by prioritizing use of weight-loss medications for members most in need, including those with severe obesity and other obesity-related comorbidities. We aim to balance access and affordability for our members and clients, and the rising costs associated with weight loss medications is impacting the affordability of health insurance for all members, not just those using therapy,” according to a statement issued by the insurer in 2024.
Representatives from the Scottdale teachers union and lawyers for the school district did not respond to requests for comment.