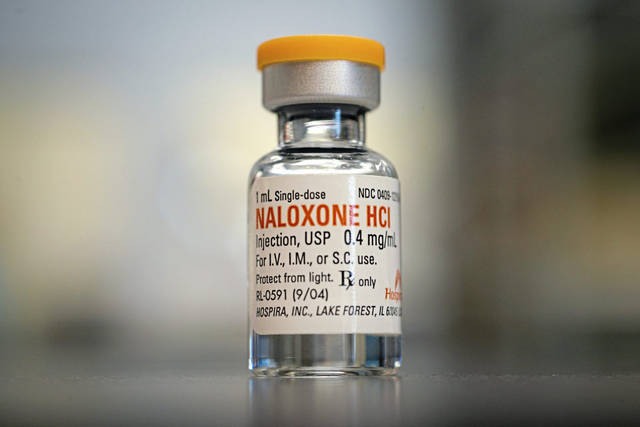
A new government report found that although naloxone prescriptions have increased substantially in recent years, prescription rates are still too low. Naloxone, a drug that temporarily reverses the effects of opioids, can help prevent overdose deaths and should be prescribed with all high-dose opioid prescriptions. According to the Centers for Disease Prevention and Control, nearly 9 million more naloxone prescriptions should have been dispensed in 2018.
Certainly patients on opioids should have access to potentially lifesaving naloxone. But shouldn’t we also consider whether those 9 million patients prescribed potentially deadly opioids are taking the wrong medicine in the first place?
The same CDC Guideline for Prescribing Opioids for Chronic Pain that recommends that naloxone be paired with opioid prescriptions also states that opioids should not be the first choice in treating chronic pain. When opioids are used for chronic pain, CDC warns against high-dose treatment, because higher doses generally increase risk without adding benefit.
In fact, there’s no evidence that supports the use of opioids for chronic pain. Opioids are vital drugs for acute trauma, surgery, cancer care and end-of-life care, and are important occasional treatments for certain recurring conditions — for example, sickle cell crisis. But daily opioid use in chronic pain patients can actually increase sensitivity to pain. So why are 9 million patients, most of whom are being treated for chronic pain, receiving 38 million high-dose opioid prescriptions annually?
One reason, not to be underestimated, is the influence of opioid manufacturers. Chronic pain treatment is the most profitable market for opioid manufacturers. While the role of opioid makers in creating the opioid epidemic has been well-documented, the current role of pharmaceutical companies in perpetuating the epidemic is less known.
Starting in the 1990s, Oxycontin and other opioids were aggressively and misleadingly marketed as effective, non-addictive treatments for chronic pain. Opioid manufacturers paid opinion leaders, medical societies and pain advocacy organizations to counteract physicians’ sensible concerns about prescribing long-term opioids, and opioid prescribing soared. The epidemic of addiction and overdose deaths soon followed.
Called out for its role, manufacturers changed course, but they haven’t stopped pushing opioids. Today’s marketing messages may be more subtle, but they are still being conveyed by paid opinion leaders and sponsored organizations, and they are still effective.
Here’s one: ”the pendulum has swung too far.“ That’s industry-speak for a campaign that holds that any restrictions of opioids harms chronic pain patients. An overcorrection, if you will. There is no evidence to support this claim. Anecdotes, yes. Evidence, no. Every evidence-based guideline, including those from the CDC, the Veterans Affairs/Department of Defense, and many states (including Oregon and Arizona), concludes that high-dose opioid prescriptions for chronic pain should be limited.
While opioid prescriptions are declining, they are still far too high, according to the CDC and many studies. High-dose opioid prescriptions should come with naloxone, but the number of people on high-dose opioids should be a small fraction of 9 million. Our goal should be to shine a light on industry influence on medical practice and to support efforts to reduce high-dose opioid overprescription for chronic pain. Reducing opioid prescriptions — and keeping them down — will reduce opioid-related addiction and death. The pendulum hasn’t swung far enough.