We are nine months into the covid-19 pandemic, with many succumbing to face covering and physical distancing fatigue, and pockets of pervasive skepticism about the virus threat and its risk. No one is happy, and everyone has someone to blame for their anger, grief and malcontent. The question people are asking is, when will the pandemic end so we can stop wearing face coverings and physically distance?
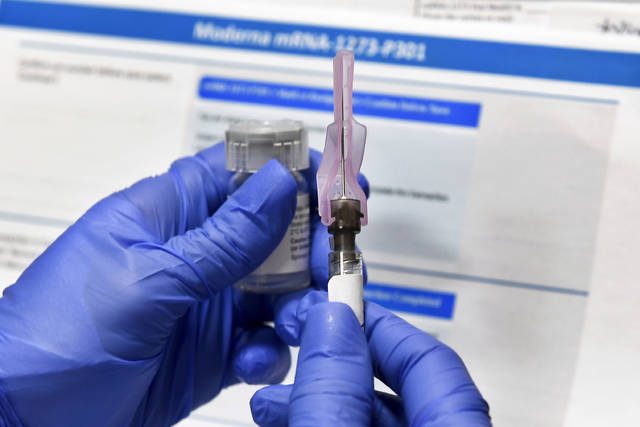
Significant investments to develop safe and effective covid-19 vaccines appear to be paying off. Recent announcements by Pfizer and BioNTech SE, Moderna, and AstraZeneca are promising. History suggests that moving such vaccines from the laboratory and into mass production and distribution may still take many more months. Challenges with the vaccine cold chain, unforeseen adverse side effects, supply chain distribution and last-mile delivery will create headwinds that have yet to be resolved. As vaccine uptake expands across the population, the rate of new infections will wane, though pockets of outbreaks will continue to occur. This means vaccines will improve significantly, but not eradicate, the current public health climate.
With more than 284,000 deaths and over 15 million confirmed cases, and at an average of well over 1 million new cases each week as we approach the new year, the summer of 2021 could take us to over 32 million confirmed cases and 500,000 deaths. Assuming seven additional infections for each confirmed case (as per CDC estimates) brings our nation to well over 60% of the US population exposed to the virus, approaching the threshold some believe that herd immunity may be realized. Will that be sufficient to slow the spread of the virus? But at what price of human carnage?
The biggest societal threat to covid-19 is not just the poor outcomes and deaths resulting from the virus, but the uncertainty of who will be the next victims of such outcomes. Age, as well as underlying health conditions like obesity, diabetes and hypertension, have been associated with poor outcomes. Conversely, CDC data indicate the vast majority of such people survive. For example, the aggregate covid-19 case fatality rate for those older than 65 is around 10%, while the 2018 general population fatality rate for this age group was 4%. Moreover, long-term sequelae (a condition which is the consequence of a previous disease or injury) of covid-19 are poorly understood but are increasingly recognized as potential concerns. The risk mitigation solution for at-risk populations is clear and simple: prevent infections.
Health care workers on the front lines need the necessary tools to perform their jobs and stay protected. If they become infected, they become unavailable to provide health care services, leading to a collapse of health care delivery systems. In addition, if they are unknowingly asymptomatic or presymptomatic yet contagious, they may infect others under their care, including highly vulnerable patients at risk for poor outcomes.
Personal protective equipment (PPE) is critical to protect health care workers and those they are treating. Yet nine months into the pandemic, N95 masks and face shield shortages continue to plague the nation’s health care system. The Biden covid-19 plan offers hope to fill this need, but it will still take many months after his inauguration to be realized. Without ample PPE supplies, the virus will continue to linger and spread, further delaying the end.
The game-changing covid-19 medical breakthrough will be the development of highly effective treatments, which is critically important and should be at the top of the list for the Biden administration. One clinical study reported that Remdesivir might not be effective in reducing fatalities, though it continues to be used with positive results.
Clearly, a major effort and investment on the treatment front is imperative. Like malaria and HIV, neither of which have vaccines but have effective treatments, the quantum leap forward for ending the social and economic scourge brought about by covid-19 lies in identifying multiple treatment vectors that eradicate the worst covid-19 outcomes. Such treatments will address the inevitable localized pockets of covid-19 outbreaks that will erupt well into 2022, and possibly beyond, particularly with vaccines that do not offer 100% immunity, with an uncertain time horizon for such protection.
With fewer sunlight hours and cooler weather, more activities are moving indoors, creating fertile environments for the spread of the virus. The light at the end of the covid-19 tunnel continues to wax and wane, seemingly extinguished at times.
The question many are asking is, when will it be reached? Adherence to CDC guidelines of wearing face coverings around other people and maintaining physical distancing buys lifesaving time. These are personal choices with societal implications.
Effective treatment, not vaccines, is the most reliable way to get us there and keep us all safe for the long run.